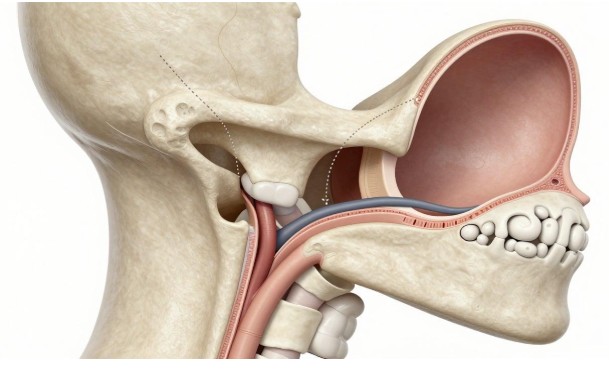
The mastoid bone sits right behind your ear. It helps with hearing by holding air cells that connect to the middle ear. When infections or growths damage it, everyday sounds can fade away. Think of it like a hidden cave system in your skull—if it gets clogged or eroded, pressure builds up and pain follows. Mastoiditis, a swelling from bacterial infections, often starts in the middle ear and spreads. Chronic otitis media, a long-lasting ear infection, can lead to holes in the eardrum or worse. These issues push many folks toward surgery to clear things out and save their hearing.
This guide breaks down mastoid surgery step by step. You’ll learn when doctors recommend it, the main techniques they use, and what results to expect. By the end, you’ll see why this procedure can turn a painful problem into a path for better ear health.
Indications for Mastoid Surgery: When Intervention Becomes Necessary
Doctors don’t rush into mastoid surgery. They watch for signs that meds alone won’t fix the issue. The mastoid air cells, those tiny pockets behind the ear, can trap infection or abnormal tissue. If ignored, damage spreads fast. Let’s look at key reasons why surgery steps in.
Chronic Suppurative Otitis Media (CSOM) with Cholesteatoma
Cholesteatoma tops the list for mastoid surgery needs. It’s a skin growth in the middle ear that acts like a slow-moving invader. It eats away at bone, including the mastoid, and can wreck nearby nerves or the inner ear balance system. Without removal, it risks hearing loss or even facial paralysis.
You might wonder: how common is this? Studies show cholesteatoma hits about 6 to 12 people per 100,000 each year in the U.S. Early surgery clears it out completely. This preserves as much hearing as possible. Patients often regain normal ear function after the growth is gone. Delaying? That just lets it dig deeper, like roots cracking a sidewalk.
For CSOM without cholesteatoma, surgery helps if the infection drains endlessly. It creates a safe, dry ear that fights off future bugs.
Chronic Mastoiditis and Intracranial Complications
Mastoiditis can flare up suddenly or linger for months. Acute cases start with fever, ear pain, and swelling behind the ear. Antibiotics work for most, but some resist. That’s when surgery drains the pus and opens the cells.
Chronic forms hide symptoms but cause steady bone loss. Left alone, infection creeps into the skull. Risks include meningitis, a brain lining inflammation, or abscesses that press on brain tissue. These emergencies demand quick action—surgery clears the path and stops the spread.
Imagine your ear as a faulty drain. Clogged mastoid cells back up the whole system. Surgery unclogs it, preventing floods upstairs in the head. Urgent cases see surgery within days to avoid lasting harm.
Management of Otosclerosis and Ossicular Chain Fixation
Otosclerosis stiffens the tiny ear bones, blocking sound waves. Mastoid surgery isn’t the first choice here, but it aids when the middle ear needs extra access. In tough tympanoplasty fixes or stapes revisions, surgeons use the mastoid route for clear views.
Ossicles—the malleus, incus, and stapes—get stuck or broken in these cases. Mastoidectomy lets doctors reach and repair them without blind pokes. It’s like opening the hood of a car for a deep engine tune-up.
This approach shines in revisions, where scar tissue clouds the field. Patients with mixed hearing loss benefit most. Surgery here boosts sound transmission, often closing the gap between what you hear through air and bone.
Surgical Approaches and Techniques in Mastoid Surgery
Surgeons pick techniques based on the problem’s size and spot. The aim stays the same: wipe out disease while sparing healthy parts. Modern tools make cuts precise, cutting recovery time. You’ll hear about open versus closed methods next.
The Canal Wall-Down Mastoidectomy (CWDM)
CWDM has roots in the early 1900s, when infections killed often. Today, it fits big cholesteatomas or blocked middle ears. Surgeons remove the ear canal’s back wall, creating one big cavity from mastoid to ear canal.
This open setup lets them scoop out every bit of bad tissue. No hiding spots left. But it means a larger hole that needs cleaning later. Patients learn to dry the area after showers to avoid new infections.
Post-op, the cavity heals into a stable space. Healing takes weeks, with packs inside to shape it. CWDM suits cases where full access trumps a tidy look.
The Canal Wall-Up Mastoidectomy (CWUM) / Modified Radical Mastoidectomy (MRM)
CWUM keeps the canal wall intact, like building a fence around the work site. It’s great for small growths or repeat surgeries. The mastoid gets opened from behind, but the ear canal stays separate.
This method cuts down on cavity care. No big open bowl to fuss over. Surgeons might add reconstruction, like fat or bone paste, to fill gaps. It preserves the ear’s natural shape and function.
MRM blends ideas—removes disease but rebuilds the wall if possible. Patients love the quicker return to swimming or showers without worry. For attic cholesteatomas, CWUM shines by hugging the disease without excess bone loss.
Techniques for Ossicular Reconstruction and Grafting
After clearing the mastoid, fixing hearing comes next. Ossicles often need swaps or bridges. Prosthetics like TORP (total ossicular replacement prosthesis) link eardrum to inner ear.
Surgeons harvest your own bone or cartilage for grafts. These blend in naturally, like patching a quilt. In CWDM, they might line the cavity with skin or muscle to speed healing.
Laser tools now vaporize tiny bits without rough drilling. This spares nerves and cuts bleeding. Results? Smoother ops and less swelling. Patients report clearer hearing soon after.
Clinical Outcomes and Postoperative Management
Surgery success hinges on quick healing and smart follow-up. Most folks walk out with less pain and better ears. But results vary by the starting damage. Let’s unpack what happens next.
Hearing Improvement and Audiological Results
Right after surgery, ears feel stuffy from packing. Hearing dips at first, then climbs. Long-term, many close the air-bone gap—the difference in sound conduction—by 10 to 20 decibels.
Factors matter: if ossicles shattered badly, gains stay modest. Stapes fixes in otosclerosis can restore near-normal levels. Studies peg 70-80% success for hearing boosts in cholesteatoma cases.
You track progress with regular hearing tests. Simple: sounds get sharper, conversations easier. Some use hearing aids short-term while nerves settle.
Disease Recurrence and Long-Term Follow-Up
Recurrence haunts cholesteatoma patients. CWDM rates hover at 5-10%, lower than CWUM’s 20% due to better access. Lifelong checks catch issues early.
Tips: Keep ears dry. Use drops if your doc says. Annual exams with scopes spot hidden spots. Audiograms measure any slips.
Sticking to this plan keeps the ear safe. One missed sign, and you’re back at square one. Most patients thrive with routine care.
Managing Postoperative Complications
Vertigo spins you for days—it’s the inner ear adjusting. Tinnitus, that ringing, ebbs over months. These fade with rest and meds.
Rarer woes hit 1-2% : facial nerve tweaks cause temporary weakness. CSF leaks, fluid from the brain, need quick seals. Infections? Antibiotics nip them.
Watch for fever or pus. Call your surgeon fast. Most issues resolve with tweaks, not big fixes. Patience pays off here.
Minimally Invasive and Emerging Trends in Mastoid Surgery
Old-school mastoidectomy works, but new ways promise less hassle. These trends cut scars and speed bounces back. Doctors test them for safety first.
Endoscopic Techniques in Middle Ear and Mastoid Surgery
Endoscopes, slim cameras on tubes, peek where drills can’t. They light up hidden corners during mastoid work. No big cuts needed for revisions.
In tight spots, like epitympanic disease, scopes guide precise snips. Patients get day surgery vibes—home same day, less pain. Visualization beats open methods for small jobs.
Adoption grows; trials show equal clearance with fewer complications. It’s like using a flashlight in a dark attic instead of knocking down walls.
Bone Preservation and Ablation Strategies
New drills and lasers zap disease while saving bone. Piezoelectric tools vibrate away soft tissue, sparing hard bone. This keeps the mastoid stronger.
Obliteration fills dead space with gels or scaffolds that regrow bone. Recovery? Faster, with smaller cavities. Emerging data hints at 90% disease-free rates.
These suit young patients or active types. Less maintenance means more freedom. Watch this space—it’s changing mastoid surgery fast.
Conclusion: Weighing Risk Against Reward in Mastoid Surgery
Choosing mastoid surgery means balancing the ear’s threats against op fixes. Pathology size, your health, and surgeon skill guide the pick—CWUM for subtle issues, CWDM for bold ones. Risks like infection weigh light against losing hearing or worse.
The win? A dry, safe ear that hears well. Collaboration counts: you follow care, your team monitors close. With that, long-term success feels real. Talk to your ENT soon if ear woes linger—early steps lead to the best outcomes
Write and Win: Participate in Creative writing Contest & International Essay Contest and win fabulous prizes.